1. Introduction
In 2022, the World Health Organization (WHO) issued a brief [1] with facts and figures showing that the COVID-19 pandemic has had a severe impact on the mental health and well-being of individuals, in particular the young. The brief further raises concern about the increase in suicidal behavior in the young under the light of the psychological post-COVID-19 society context producing ontological fears and insecurities in individuals worldwide. In the wake of the pandemic in 2022, WHO experts worldwide witnessed a significant rise in mental health issues, anti-depressant prescription uptakes, and an increase in suicide statistics in young individuals. In France, for example, a significant increase in medical consultations for suicidal behaviors and thoughts associated with anxiety and depression among 18–24 year-olds, with a peak in 2021 after the first waves of the COVID-19 pandemic, was revealed by the 2021 public health barometer survey statistics [2] relative to the prevalence of generalized anxiety disorder (GAD) and depression with suicidal ideation in the global national population. Before the COVID-19 pandemic, anxiety in the young received already some attention from scientific studies [3]. The first-ever large-scale meta-analysis of cross-sectional studies on the global prevalence of GAD among medical students [4] suggested a global prevalence rate of anxiety in this population of about 33.8% across the globe. Anxiety was more prevalent among medical students from the Middle East and Asia by comparison with Western countries. Analyses for gender produced no statistically significant difference [4]. Since then, further reports on raised anxiety levels and their short- and long-term consequences affecting young individuals worldwide have been made public and subject to large-scale meta-analysis [5]. Epidemiological studies on children, adolescents, and individuals younger than 24 across digital databases worldwide suggest that youth with mental health and learning disabilities diagnosed before the pandemic were potentially more vulnerable to experiencing anxiety disorders during the pandemic [5]. Standardized mean differences (SMD) between prevalence ratios (RR) for anxiety in pre- and post-COVID-19 pandemic context [6] show that the SMD for post-COVID-19 anxiety scores had significantly increased by 2021 compared with scores from the pre-COVID-19 period. Students, and medical students in particular, who manifest higher baseline rates of anxiety compared to the general population and their age-matched peers at any time [7], have been reported to suffer from COVID-19 pandemic-related anxiety for reasons beyond the academically and emotionally demanding training constraints [8, 9]. Student distress and untreated anxiety not only negatively impact academic performance but also incur a personal cost, given that anxiety is associated with reduced quality of life [10], loss of relationships [11], and heightened risk of depression and its consequences [12]. Meta-analysis of the literature has led to estimates of anxiety prevalence in 38–50% of medical students during the COVID-19 pandemic with variable socio-demographic correlates, with higher rates for medical students in the Eastern Mediterranean Region (EMR) compared to other WHO regions [6]. Some studies revealed higher levels of anxiety in female Saudi, Brazilian, and Iranian medical students compared with the male population [13–15]. The present survey was conducted in 2022 in a context where the COVID-19 pandemic was transitioning into the endemic phase [16] as a result of massive vaccination programs worldwide that had permitted gaining some level of control over the then predominant pervasive Omicron variant. The study goal was to assess the relative severity of psychological and somatic symptoms of anxiety in a population of undergraduate medical students at Strasbourg University, France, in the post-COVID-19 social context in 2022. During the pandemic and in particular the lockdown periods, all students had received considerable support from Strasbourg University, both in terms of psychological support, operational 24 hours a day through a telephone and online crisis center that had been rapidly put in place for them, and in terms of material support. Emergency food supplies were made available for little if any cost, by the University as well as by privately run initiatives, and punctual financial support was granted by the University to students in difficulty during that time. The teaching staff was repeatedly instructed to keep in touch with their students and to exchange online with them as much as possible. Results from a post-pandemic survey [17] suggest that the quality of the University support provided by administration and instructors during the COVID-19 pandemic has played an important role in modulating the extent of COVID-19-induced stresses and their impact on successful degree completion and individual levels of students’ well-being.
2. Materials and methods
2.1. Study scope
Punctual states of anxiety are a normal response of the organism to acute stress, with adaptive effects such as increased attention and focus on a specific task, for example. By contrast, GAD differs from such temporary anxiousness or nervousness, with a more intense and diverse set of psychic and somatic manifestations of restlessness, worry, and fear. The Diagnostic and Statistical Manual, Fifth Edition (DSM-5) describes GAD as excessive worry and apprehensive negative expectations or fears occurring more often than not for at least six months [18]. In clinical observations, this syndrome is frequently associated with at least three or more of the following symptoms, present more often than not in the individual’s daily life: restlessness, fatigue, difficulty concentrating or mind going blank, irritability, depressed moods, anhedonia, muscle tension, tension headaches, disturbed sleep, genito-urinary troubles, and digestive problems, causing clinically significant distress and impairment of social, occupational, and other important aspects of normal functioning in daily life. To assess the severity of both psychological and somatic symptoms of GAD in a population of undergraduate medical students at the University of Strasbourg in the wake of the COVID-19 pandemic in 2022, we implemented an online version of the well-established and widely used Hamilton Anxiety (HAM-A) scale [19]. A link to the survey was sent to several hundreds of individuals (the QR code of the online test may be obtained upon request). Eighty medical undergraduates spontaneously took the survey on a voluntary basis.
2.2. The Hamilton Anxiety Scale (HAM-A)
The HAM-A was one of the first clinical tests developed to measure the severity of GAD and is widely used in clinical contexts and in research projects on adults, adolescents, and children. The time frame for symptoms concerns the past six months. The score of the relative severity of symptoms from 0 to 4 is to reflect the extent to which they interfere with the individual’s daily life and well-being. The average time needed to complete the test online is about 20 minutes. It consists of fourteen items, or test questions, where each of them refers to a set of symptoms (Table 1). Each of the fourteen test questions or items is scored on a scale between “0” and “4”, where “0” stands for “no symptoms present”, “1” for “mild symptoms”, “2” for “moderate” symptoms, “3” for “severe” symptoms, and “4” for “very severe” symptoms. The total of an individual test score varies between 0, in which case a “0” was scored in response to each of the 14 questions or items, and 56, in which case a “4” was scored in response to each of the 14 items. A total test score lower than 17 indicates an anxiety syndrome of mild severity, and a score between 18 and 24 indicates anxiety of mild to moderate severity. Total scores between 25 and 30 indicate moderate to severe anxiety, and totals higher than 30 indicate a very severe anxiety syndrome. While the total score does not deliver detailed insight into the relative weight of psychological symptoms of anxiety (fearfulness, mental agitation, psychological distress, etc.) and somatic symptoms (abdominal pain, muscle tension, headaches, etc.), the comparative analysis of scores in response to psychological (test items 1–6) versus somatic symptom-related test questions permits such, as will be shown further below.
Table 1
Symptoms of generalized anxiety disorder probed by each of the 14 test items/questions of the Hamilton Anxiety Scale
2.3. Participants
About 200 potential undergraduate participants received the link to the survey form with an informed invitation to participate anonymously. It was explicitly stated in the invitation that participants willing to take the survey had to be in good general health and not to be under, or considered for, treatment of a specific physical or mental condition. The 80 participants who accepted the invitation remained anonymous but were assigned an individual ID number when starting to pass the test online. They were prompted to enter information relative to age and gender before receiving more specific instructions for taking the HAM-A online. Participants’ age varied within the range from 18 to 24 years. In total, 57 of them self-identified as “female”, 20 as “male”, and 3 as “non-binary”.
3. Results
Individual test scores in response to each of the fourteen test items were computed and submitted to descriptive as well as statistical analyses.
3.1. Global scores
In the first step, the severity of GAD in individuals, based on their global test scores, was assessed. Findings show that 40% of the participants produced global test scores between 12 and 17 revealing mild generalized anxiety, 24% produced scores indicating moderate generalized anxiety, 24% produced scores indicating severe anxiety syndrome, and 12% produced scores indicating very severe generalized anxiety. The percentages are shown graphically in Figure 1. These results indicate that about a third (36%) of the sample population displayed a severe to very severe generalized anxiety syndrome according to the HAM-A score in 2022.
3.2. Item-based analysis
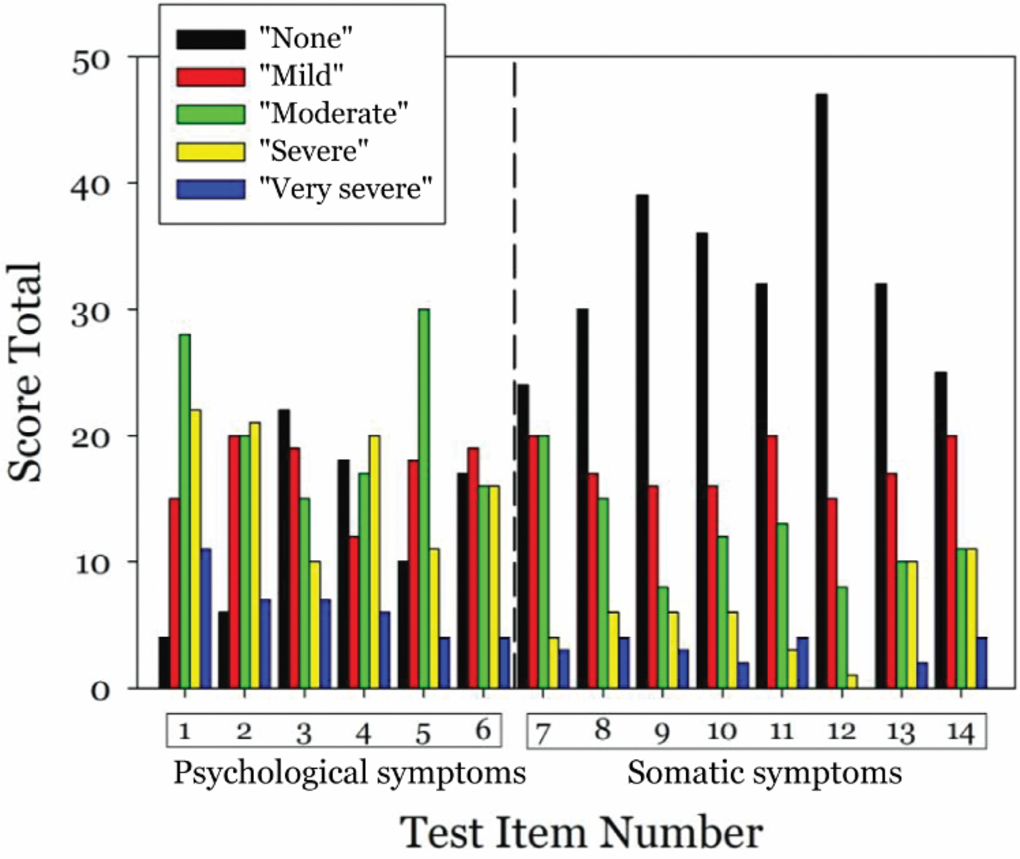
In the next step, the total scores for each of the fourteen items (test questions) of the HAM-A were analyzed as a function of the severity category they reflect. Figure 2 shows these results graphically. The totals per severity category display clear differences when comparing scores for items relating to psychological symptoms (items 1–6) to scores for items relating to somatic symptoms of GAD (items 7–14). Higher score totals for the categories “moderate”, “severe”, and “very severe” and markedly lower scores for the category “none” are observed for psychological symptoms (items 1–6) by comparison with somatic symptoms (items 7–14).
3.3. Analysis of variance
Given the marked differences between scores for items relating to psychological symptoms and items relating to somatic symptoms of GAD, analysis of variance (two-way ANOVA) was performed comparing scores for items 1–6 to scores for items 7–12 to assess statistical significance. Score totals for test items 13 and 14 were excluded from this analysis to allow for two-way ANOVA under the general linear model assumption, which requires an equal number of data (n) per factor level. The analysis plan therefore corresponds to a Cartesian Design I2 × S5, with two levels of the item (I) factor (“psychological” vs. “somatic”) and five levels of the severity (S) factor (“none” vs. “mild” vs. “moderate” vs. “severe” vs. “very severe”) on six (n) raw data points in terms of score totals per combination of factor levels for a total (N) of 60 data with 59 (N − 1) degrees of freedom (DF). The results of this analysis show a significant effect of the item (I) factor with F (1, 1) = 4.45; p < 0.05, a significant effect of the severity (S) factor with F (1, 6) = 18.21; p < 0.001, and a significant interaction between the two factors with F (1, 6) = 15.10; p < 0.001. Given the significant interaction, post-hoc tests (Holm-Sidak) were performed to assess the significance of the different factor level combinations. These analyses show a significant effect of item (I) for the level “none” of severity (S) with a difference (d) between means of d = 21.80 and t (1, 1) = 7.75, p < 0.001; no effect for the level “mild” with d = 0.16 and t (1, 1) = 0.06, NS; a significant effect for the level “moderate” with d = 8.33 and t (1, 1) = 2.96, p < 0.05; a significant effect for “severe” with d = 16 and t (1, 1) = 3.28, p < 0.01; and no effect for “very severe” with d = 4 and t (1, 1) = 0.82, NS. The interaction between item type (“psychological” vs. “somatic”) and severity is shown graphically in Figure 3.
Figure 3
Total scores for regrouped test items/questions of the Hamilton Anxiety Scale for psychological (items 1–6) and somatic symptoms (items 7–12) as a function of the category reflecting their severity for significant interactions between factor levels within the linear model (two-way ANOVA). The error bars reflect the standard errors of the means (SEM).

4. Discussion
The findings indicate that 60% of the sample population from this study manifest moderate to very severe GAD based on their HAM-A test scores, and 36% a severe to very severe syndrome in the post-COVID year 2022, in a context where a lot was done by the university and individual stakeholders to provide financial as well as psychological support to students during the pandemic. These percentages are similar to those identified in results from larger, cross-sectional studies performed in the same year in other countries and contexts, where 30% or higher prevalence of anxiety was found in student populations [6, 13, 20]. In these studies, left-behind status, lower economic status, traumatic experiences, exposure to the pandemic, and rumination due to social isolation during the lockdown period could be identified as risk factors of anxiety and psychological distress in the young. Unfortunately, this kind of background information is available for this study here, which is a limitation for the interpretation of the findings. However, it was found previously that lack of academic satisfaction is correlated with anxiety and psychological stress in students [5, 6, 21], urging institutions and universities to address factors that help maximize students’ academic satisfaction in addition to ensuring that they have access to psychosocial services that help them cope with psychological distress. The novelty of the findings from this study here is that they show a statistically significant difference between psychological and somatic symptoms of GAD, with a significantly higher prevalence of psychological symptoms in the sample population here. Results from a large cohort study in the United Kingdom [22] showed that moderate to high levels of anxiety directly associated with the COVID-19 pandemic in 2020 were significantly associated with somatic symptoms characteristic of GAD, in particular with gastrointestinal and fatigue symptoms. This pattern of association remained significant after controlling for psychological symptoms of GAD, pre-existing health problems, age, gender, and income. Specific fears and anxiety directly associated with COVID-19 during the pandemic therefore made a unique contribution to somatization above and beyond GAD. We may therefore suggest that the anxiety scores found in the population from this study here do not necessarily, or not only, reflect a consequence of the COVID-19 pandemic, but a more sustained problem of the young. Another limitation of the present study relates to the fact that anxiety is viewed through a pinhole here in the example of a relatively small population of medical students in France, where particularly high demands are placed on them in a competitive academic context. Anxiety problems already started rising in children and youth before the pandemic [23], with a 151% increase in mental health concerns in children as young as 10–14, with anxiety as a common denominator. In France, national statistics made available by Santé Publique France in 2023 [24], clearly show that the mental health of youth in France has deteriorated considerably in the past two years. This deterioration is particularly prevalent among adolescents aged 11–17 and in young adults aged 18–24, the same age range as that of the study population in this work here. In addition, reported use of emergency care for mood disorders, suicidal ideation, and gestures increased sharply in 2021 and 2022 and has remained at its highest level ever since [24]. Among young people aged 18–24, this increase has continued markedly in the year 2023. It is stated further that 20.8% of 18–24 year olds were affected by depression in 2021 compared to 11.7% in 2017. Finally, among 17-year-olds, 9.5% were affected by severe anxiety-depressive symptoms in 2022 compared to 4.5% in 2017, and 18% had suicidal thoughts during the year compared to 11% in 2017. In September 2023, visits to the emergency room for suicidal gestures and thoughts, mood disorders (depressive episodes in particular), anxiety disorders, and medical interventions for anxiety increased among children in the age range between 11 and 17. In this recent context of record statistics for mental health issues in young individuals, complex problem spaces where long hours spent in front of blue-light emitting computer screens [25], often combined with digital addiction, sleep dysfunction [26], and other internet-mediated mental health issues in students [27, 28], have been identified. Finally, although there is a large amount of research on anxiety and related psychological problems linked to the COVID-19 pandemic timeframe, at this stage it is not clear what the potential solutions of this could be. Stressors in university life have been positively associated with anxiety symptoms in students [29], and future research should focus more on potential solutions to alleviate these stresses. Studies on student anxiety in the critical time frame considered, as meta-analysis had shown [30] used self-report methods to assess anxiety scores, a limitation the present study here shares with the others. Clinicians or mental health experts were not asked to evaluate the psychological status of the participants in terms of third-party verification, and more clinical as well as experimental research is urgently needed to shed light on causal links, and to find support solutions helping youth to find balance in a troubled world.
5. Conclusions
The results here offer a pinhole view of GAD in the post-COVID-19 year 2022 in a sample population of medical students at a French university. In total, 36% of that population displayed severe to very severe GAD, with a relative predominance of psychological symptoms by comparison with somatic symptoms. The findings suggest that student anxiety needs to be tackled in terms of a larger societal problem not reducible to the immediate consequences of the pandemic per se, reaching further and far beyond and urgently calling for more research into causal links.